 Decades ago in veterinary medicine, pain was thought to be good for an injured or sick animal. This wasn’t because veterinarians were cruel or wanted pets to suffer; they believed that pain helped keep animals sufficiently quiet in order to heal. Plus, it was thought that there really wasn’t any way to know whether a pet was feeling pain or needed some relief. Today it’s just the opposite: veterinarians now believe they should treat for pain until there is proof that an animal isn’t hurting.
Decades ago in veterinary medicine, pain was thought to be good for an injured or sick animal. This wasn’t because veterinarians were cruel or wanted pets to suffer; they believed that pain helped keep animals sufficiently quiet in order to heal. Plus, it was thought that there really wasn’t any way to know whether a pet was feeling pain or needed some relief. Today it’s just the opposite: veterinarians now believe they should treat for pain until there is proof that an animal isn’t hurting.
Why it’s important to manage your pet’s pain?
Pain management has become an important issue in veterinary medicine. AAHA along with the American Association of Feline Practitioners recently released the AAHA/AAFP Pain Management Guidelines for Dogs and Cats . These guidelines show that pain management will improve the recovery process, whether from illness, surgery or injury. Best of all, because it reduces stress and increases a sense of well being, pain management may even help your furry friend live longer.
Different kinds of pain
Acute pain comes on suddenly as a result of an injury, surgery, inflammation or infection. It can be extremely uncomfortable for your pet and it may limit her mobility. The good news is that it’s usually temporary. It generally goes away when the condition that causes it is treated.
Chronic pain is long lasting and usually slow to develop. Some of the more common sources of chronic pain are age-related disorders such as arthritis, but it can also result from illnesses such as cancer or bone disease. This pain may be the hardest to deal with, because it can go on for years, or for an animal’s entire lifetime. Also, because it develops slowly, some animals may gradually learn to tolerate the pain and live with it. This can make chronic pain difficult to detect.
How to know when your pet is hurting?
When we have pain, we complain. However, animals instinctually hide pain so we generally don’t hear a peep out of our pets until the pain is so bad they cannot hide it anymore. So how do you know when your pet’s in pain?
Because our furry friends aren’t able to tell us when something is wrong, it’s important for you, the owner, to take note of any change in their behavior. Look for any of the following signs they may be your pet’s way of saying “I hurt.”
- Being unusually quiet, listless, restless, or unresponsive
- Whining, whimpering, howling, or constantly meowing
- Biting
- Constantly licking or chewing at a particular part of the body
- Acting funny and out of character, either aggressively or submissively
- Flattening ears against the head Having trouble sleeping or eating
- Seeking a lot more affection than usual
- Unable to get comfortable (constantly changes positions to find the most comfortable position)
If you suspect your pet might be hurting, consult your veterinarian for help. Your veterinarian will help you figure out the problem and discuss the available options. Be prepared to answer questions about your pet’s behavior, activity level and tolerance for being handled. Your furry friend’s mobility is also a crucial topic. Does Rover now have a hard time getting up or walking up/down stairs (these were never a problem before)? Does Fluffy no longer jump up on to the furniture or have a hard time hopping back down?
Many animals, especially cats, naturally disguise signs of pain to protect themselves from predators. However, the lack of obvious signs does not mean they aren’t experiencing pain. If the injury, illness or experience is one that sounds painful to you, go with the assumption that it may also hurt your pet and get to your veterinarian.

 Animal Health Week is a national public awareness campaign organized by the Canadian Veterinary Medical Association and hosted by veterinarians across Canada. Each year, during the first week of October, veterinarians and veterinary hospitals across Canada promote animal health and responsible animal ownership as part the of the Animal Health Week celebrations. The campaign slogan this year is ” Their health in your hands” and is centered around the benefits of preventative health care for your pets and other animals.
Animal Health Week is a national public awareness campaign organized by the Canadian Veterinary Medical Association and hosted by veterinarians across Canada. Each year, during the first week of October, veterinarians and veterinary hospitals across Canada promote animal health and responsible animal ownership as part the of the Animal Health Week celebrations. The campaign slogan this year is ” Their health in your hands” and is centered around the benefits of preventative health care for your pets and other animals.


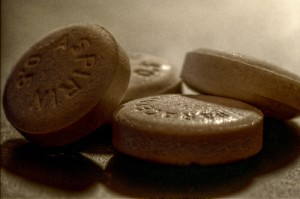 Over the counter pain medications (OTC), such as Motrin, Advil, Aspirin or Tylenol, are familiar products found in most Canadian homes. People are comfortable following the instructions for these products relating to quantity, timing, and administration of the medication. Owners with a pet that is experiencing pain may be tempted to medicate the pet with one of these products. The following discussion explains the reasons to avoid OTC pain medications in pets and why you should consult with your veterinarian.
Over the counter pain medications (OTC), such as Motrin, Advil, Aspirin or Tylenol, are familiar products found in most Canadian homes. People are comfortable following the instructions for these products relating to quantity, timing, and administration of the medication. Owners with a pet that is experiencing pain may be tempted to medicate the pet with one of these products. The following discussion explains the reasons to avoid OTC pain medications in pets and why you should consult with your veterinarian. Choosing a pet food can seem like an overwhelming task when the market is saturated with companies and products. Pet food companies skillfully use marketing techniques to promote their brand. This is a brief introduction to understanding the information presented on commercial pet foods.
Choosing a pet food can seem like an overwhelming task when the market is saturated with companies and products. Pet food companies skillfully use marketing techniques to promote their brand. This is a brief introduction to understanding the information presented on commercial pet foods. Many of our four-legged friends love a quick dip in the water on a warm day. However, pet owners should be aware of a potential danger – blue-green algae. Blue-green algae is comprised of a photosynthetic bacteria, that grows in the water, known as cyanobacteria
Many of our four-legged friends love a quick dip in the water on a warm day. However, pet owners should be aware of a potential danger – blue-green algae. Blue-green algae is comprised of a photosynthetic bacteria, that grows in the water, known as cyanobacteria

 Treatment of a porcupine encounter requires the removal of the quills ideally as soon after the incident as possible. Porcupine quills cause immediate trauma to the structures they penetrate resulting in pain and inflammation. Since dogs approach porcupines face first, often with open mouths, the majority of quills are found on the head, neck and inside the mouth. The quills can migrate within the body over time if not removed. In the region of the head and neck this may affect the eyes and brain of the animal. Quills located further from the head can also pose a threat to thoracic and abdominal organs. It is therefore important to seek veterinary care to locate and remove quills.
Treatment of a porcupine encounter requires the removal of the quills ideally as soon after the incident as possible. Porcupine quills cause immediate trauma to the structures they penetrate resulting in pain and inflammation. Since dogs approach porcupines face first, often with open mouths, the majority of quills are found on the head, neck and inside the mouth. The quills can migrate within the body over time if not removed. In the region of the head and neck this may affect the eyes and brain of the animal. Quills located further from the head can also pose a threat to thoracic and abdominal organs. It is therefore important to seek veterinary care to locate and remove quills.